
What if you were told to “just live” with an incurable and overwhelmingly painful condition? What if that condition occurred at random and through no fault of your own? And, what if we told you that though science has acknowledged its existence for over a century, the condition has remained largely ignored by global research funding?
I reckon you’d be fuming; just like the ~190 million women globally, who suffer from endometriosis. And for good reason too. For too long women have had to bear the complications of endometriosis without hope of effective medical management, due to social ignorance and inadequate research funding. What we deem as regular period pains are in fact, much, much worse for those with endometriosis, and despite decades of awareness of the condition, treatment development has been painfully slow. The impact of endometriosis remains invisible to the world for the millions of women it affects, but there are steps we can take to combat this medical discrimination for the future of women’s health.
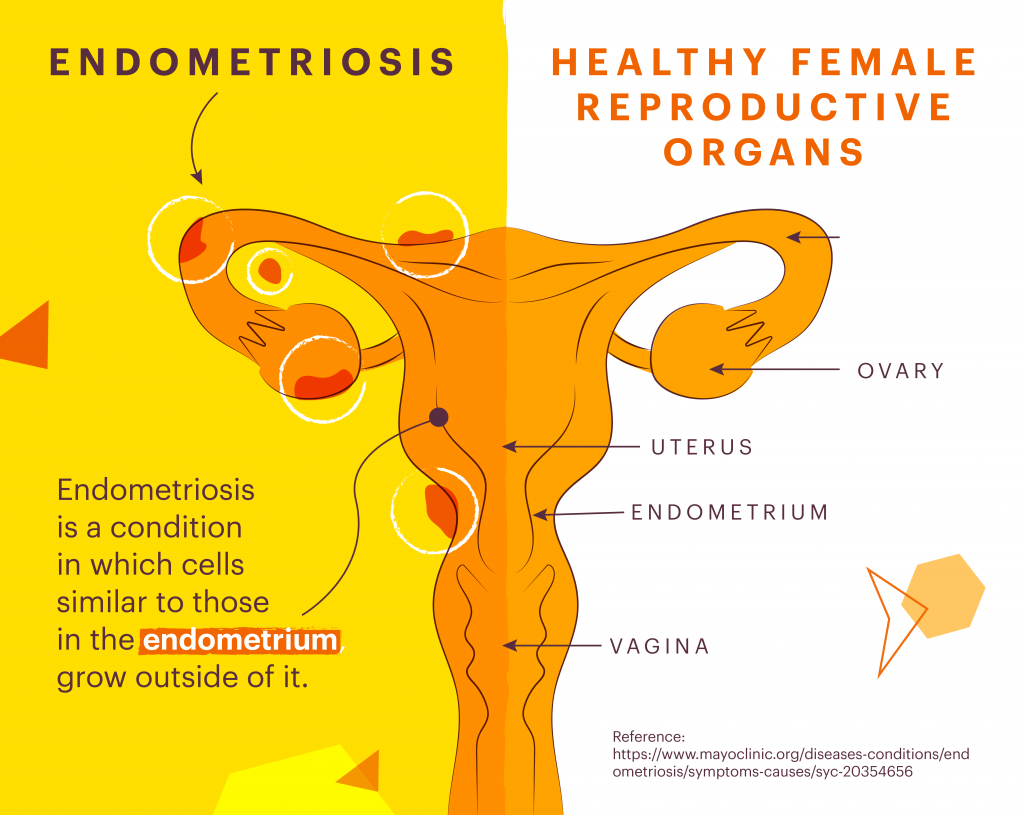
Endometriosis is a chronic inflammatory condition that has been referred to as ‘the missed disease’ due to its unclear pathophysiology and lack of consistency in its diagnosis and management. Endometriosis can affect women with wombs, and is characterised by the abnormal growth of endometrial tissue (which is meant to line the womb), in other places outside of the womb, including the ovaries and the fallopian tubes.
Each month these cells behave in the same way to those in the womb. However, unlike menstrual blood, which comprises of the endometrial tissue that leaves the body during a period, endometrial tissue formed outside the womb has nowhere to go. This can lead to inflammation and scar tissue that can cause significant pain in many women. Unfortunately, the exact cause of endometriosis remains unknown, and so we’re left looking at the condition as a cluster of pain symptoms.
The symptoms of endometriosis manifest in a way that can adversely affect an individual’s quality of life, social participation, and academic and professional productivity, such as, but not limited to: chronic pelvic pain, painful periods, painful intercourse, and infertility. For some women, these symptoms can be more pronounced, proving to be a burden on health-related quality of life.
Periods are natural. They can be painful and inconvenient. But periods for those with endometriosis can be far more painful and can lead to numerous complications. Endometriosis can reduce the likelihood of getting pregnant, and long delays in diagnosis can lead to abnormal cyst growths, surgical complications, and bladder and bowel problems, all of which may be more prevalent if there is a delay in the initiation of appropriate treatment.
Living with endometriosis may be frustrating; because friends, family, and even doctors may not take the pain seriously. We’re taught to think that period pain is something women put up with simply for being women; yet at times, the pain can be so harsh that it interferes with productivity and daily living. For instance, somebody with endometriosis may set out to do their food shop for the week and sort their ‘life admin’ but, when greeted by severe abdominal pain and cramps, they may feel more inclined to stay home, and perhaps test out a cocktail of remedies to ease their symptoms.
Women who have endometriosis may find themselves having to miss days from work because of their pain. In one 2010 survey, 85% of women stated that endometriosis interferes with their quality of work; 20% were unable to work at all; and more than two thirds, would work despite persistent pain. This endometriosis-induced absenteeism can not only result in a loss of productivity, but also lead those affected with endometriosis to feel guilty towards their colleagues. Additionally, women may not feel inclined to inform their employers of their condition, due to possible tensions and implications that may arise for them.
As such, endometriosis sufferers may find it difficult to find joy in the simplest of daily activities, due to the anxieties attributed to the disease’s complications and management. And we must not forget about the burden endometriosis has on a woman’s sexual life. Unwelcome pain during sex can lead to feelings of guilt and insecurity and can also give rise to relationship problems, particularly if the person affected by endometriosis consequently experiences fertility issues.
Endometriosis’ impact on all aspects of daily life poses a psychological challenge for affected individuals. Sufferers report feelings of anxiety and depression, which at high levels could amplify the severity of the pain felt. For this reason, it isn’t unjust to categorise endometriosis as a dastardly disabling condition that can compromise pretty much all aspects of life.
Since medicine began to understand its manifestation in 1921, endometriosis has remained a much-disputed condition. Diagnosis of endometriosis remains slow and problematic, with sufferers facing an average of 7.5 years between seeing a doctor and receiving a diagnosis; subsequently leading to longer delays in acquiring treatment and an increased risk for the development of complications.
The failure to diagnose endometriosis can be linked to a wider framework of historically outdated ideas relating to women’s health, whereby the male sex has been used as a standard of what constitutes health, and illnesses of women’s health have been systematically and historically dismissed or ignored. Beliefs dating back to the late twentieth century, that those suffering from endometriosis were older, working women, lead to the myth that only women in their 30s and 40s could develop the disease. These misconceptions led to the practice of routinely advising women to try to have children so that they might reduce their symptoms (because the absence of menstruation reduces symptoms) of endometriosis.
Female research has demonstrated that societal values are influential in the way that symptoms are interpreted and responded to, and women are consistently being trivialised, dismissed, or even misdiagnosed when presenting with symptoms of endometriosis. There is a need for comprehensive interdisciplinary approaches to managing endometriosis and to raising disease awareness for both the public and healthcare professionals. We need to remove stigma associated with periods, and allow for funds that bring to us timely diagnoses and effective treatments.
Uncertainty as to the reasons why it occurs, and difficulty in the management of endometriosis have a significant impact on the life of those living with the condition. We must look beyond traditional misconceptions surrounding period pain and menstrual bleeding as conditions women just “have to deal with”, and instead work on enhancing cooperation between healthcare professionals and patients for better understanding. And, despite there being more promising research emerging, we also need to work on improving society’s awareness of endometriosis to truly combat the stigma behind devaluing women’s pain.